G.KRUPALATHA. HALL TICKET NO: 1601006060. LONG CASE.
This is an online E log book to discuss our patient\"s de -identified health data shared after taking his/her/guardian\"s signed informed consent. Here we discuss our individual patient\"s problems through series of inputs from available global online community of experts with an aim to solve those patient\"s clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
HALL TICKET :1601006060.
A 45 year old male resident of Nalgonda labourer by occupation presented to our opd on 20 april with chief complaint of :
. Pedal edema since 15 days
. Oliguria since 15 days
. Burning micturition since 10 days
. Fever since 10 days
• shortness of breath since 8 days
• Cough since 8 days
History of presenting illness :-
Patient was apparently asymptomatic 15 days ago,then developed —
• Bilateral pedal edema, since 15 days which in insidious in onset , gradually progressed up to the thighs, pitting type , no aggravating and no relieving factors
. Decreased urine output since 15 days.
. There is history of fever since 10 days which is insidious in onset , intermittent , not associated with chills and rigors , headache , vomiting .
.History of burning micturition and oliguria since 10 days
. Shortness of breath since 8 days which was insidious in onset, non progressive, aggrevating by walking and sternous work and relieved by taking rest.
( Grade lll ).
He has history of orthopnea.
There no history of PND.
.Dry cough :-
He has dry cough since 8 days, which is insidious in onset, non progressive, no aggrevating and relieving factors.
. His appetite has decreased.
• There is no history of sweating , palpitations , chestpain , hematuria
* patient underwent 2 sessions of Dialysis after admitting in our hospital.
Past history
• 2 years back he developed symptoms of productive cough and fever for 1 week for which he visited to hospital and diagnosed with Tuberculosis and took antitubercular drugs for 6 months and at that time he was told be having some kidney issues and used some medications ( records notavailable ) .
• Not a known case of diabetes ,hypertension,asthma , convulsions
• Surgical history is not significant.
Family history
Not significant
Personal history
• decreased appetite
• Mixed diet
• Regular bowel habits and normal
• Patient has oliguria and burning micturition
• He is an alcoholic since 10 years , drinks once weekly
• Smoker since 25 years , he smokes daily 2-5 beedis
GENERAL EXAMINATION
Patient is conscious coherent and cooperative , moderately built , moderately nourished
⁃ Presence of pallor
⁃ No icterus , no cyanosis, no clubbing ,no pedal edema
⁃ No generalized
Vitals
⁃ Pulse taken in sitting position ,left radial pulse ,Pulse rate : 80bpm , regularly regular
⁃ Bp 130/80 mm hg measured in sitting position on right upper arm
⁃ Respiratory rate : 20cpm
⁃ Afebrile
RESPIRATORY SYSTEM EXAMINATION
Patient is examined in supine aswell as in sitting positions under well ventilated room with consent taken
Upper respiratory tract :
nose , oral cavity are examined and no abnormal findings are present
examination of chest proper :
- Inspection
⁃ shape of chest : normal
⁃ Symmetry of chest : symmetrical
⁃ Trial sign negative
⁃ Movements of chest : RR -20cpm . .
Type - abdomino thoracic.
. Equal on both sides
⁃ No involvement of accessory muscles and no intercoastal tenderness
⁃ No visible scars , no sinuses , no engorged veins
⁃ No deformities of spine
⁃ No visible apical impulse
- palpation
⁃ No tenderness and no local rise of temperature
⁃ Inspectory findings are confirmed
⁃ Trachea central
⁃ Apex beat : felt at 5 th Intercoastal space lateral to mid clavicular line
⁃ Decreased chest expansion
⁃ Vocal fremitus : decreased at infra axillary and infra scapular areas on both sides normal on supra clavicular, infraclavicular ,mammary , infra mammary , suprascapular and interscapular areas
- Percussion
- Direct percussion: resonant on clavicle , sternum
2. Indirect percussion :
Anterior :
⁃ resonant in supra clavicular area
⁃ Resonant in infraclavicular area
⁃ Resonant in inframammary area on both sides
⁃ Traube’s space:dull
Posterior :
⁃ Resonant in suprascapular area
⁃ Resonant in interscapular area
⁃ Dull in Infrascapular area on both sides
- Auscultation
⁃ Bilateral air entry present
⁃ Normal vesicular breath sounds heard
⁃ Reduced in B/ L infrascapular and infra axillary areas
- fine crepts heard on B/L infra axillary and infra scapular areas
CVS EXAMINATION
⁃ S1 s2 heard
⁃ No murmurs
⁃ No palpable thrills
ABDOMINAL EXAMINATION
Scaphoid shape
No tenderness
No palpable mass
No hepatosplenomagaly
No ascites
Bowel sounds present
CNS EXAMINATION
⁃ Conscious and alert
⁃ Normal gait
⁃ Normal speech
⁃ No signs of meningeal irritation
⁃ Cranial nerves , motor system , sensory , glasgowcoma scale normal
⁃ Reflexes : superficial and deep tendon reflexes are intact
Provisional diagnosis :
ACUTE ON CHRONIC RENAL FAILURE with past history of pulmonary TUBERCULOSIS .
INVESTIGATIONS
⁃ CBP
⁃ CUE
⁃ ABG
⁃ RFT
⁃ LFT
⁃ PT
⁃ APTT
⁃ Blood sugar
⁃ ESR
⁃ Serum pottasium
⁃ Blood culture
⁃ Chest x ray
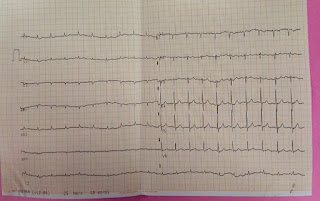
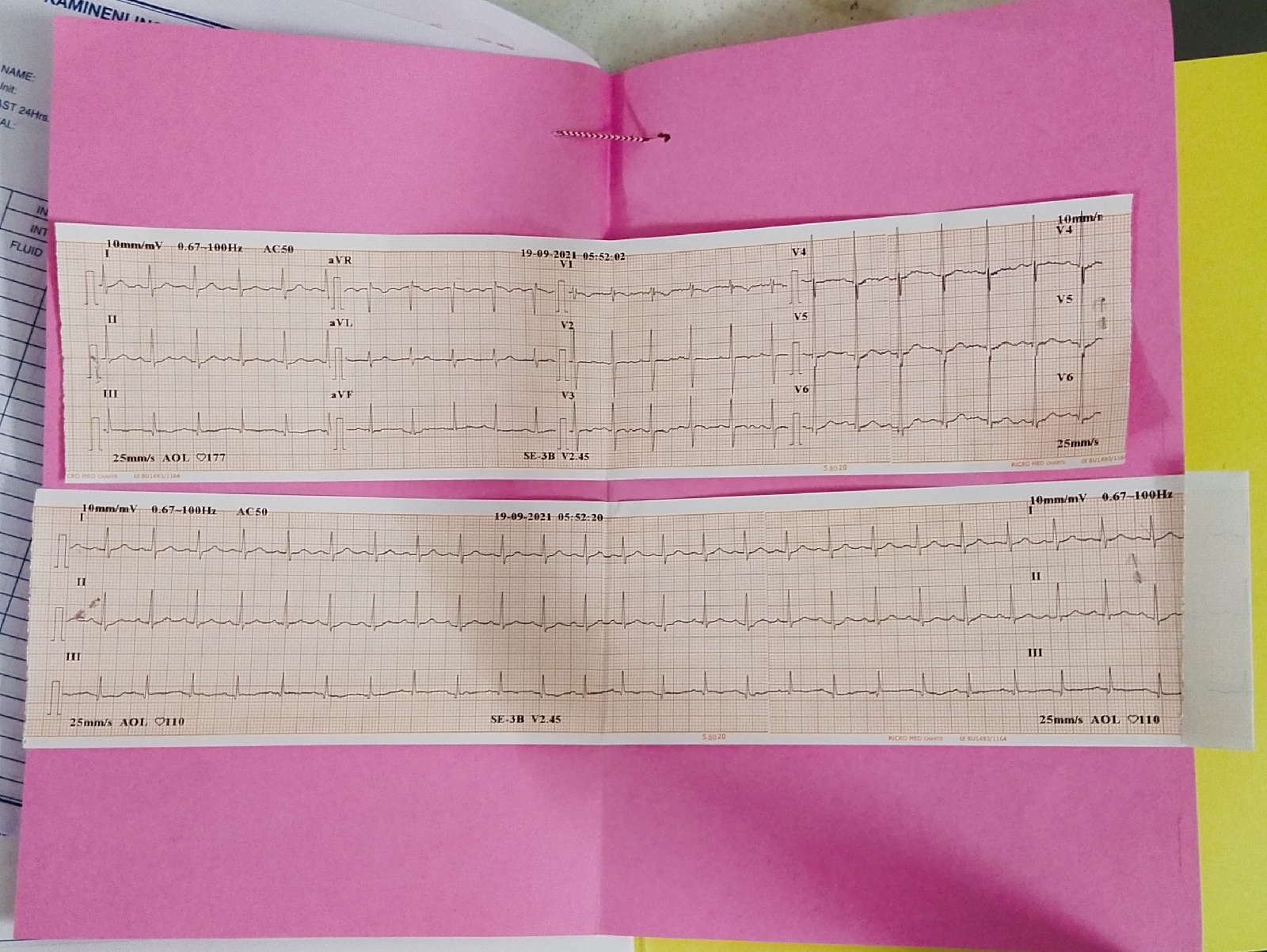
⁃ ECG
⁃ Ultrasound abdomen
TREATMENT
⁃ Salt and fluid restriction
Salt - < 2 g/ day
Fluid - < 1 lt / day
⁃ Injection iv LASIX 40mg BD
⁃ Tab NODOSIS 500mg bd
⁃ Tab SHELCAL 500mg od
⁃ Input and output charting
⁃ Nebulization with mucomist and BUDICORT 12 th hrly


















Comments
Post a Comment