72 yr old female with fever, vomitings and loose stools.
This is Online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent .Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
Case:-
Fever :
Low grade, intermittent, not associated with chills and rigors , associated with decreased Appetite, loose stools and vomiting.
Vomitings:-
3-4 episodes per day, non - bilious , non - projectile, food/ water as content.
Stools:-
10-12 episodes/day, green in colour associated with lower abdominal pain- diffuse, squeezing type, no aggrevating and relieving factors.
Patient was apparently asymptomatic 6 months back, from then she decreased using her left lower limb , walking with support (with wall/ stick).
She had intermittent episodes of vomiting since 6 months.
No bowel and bladder involvement.
K/c/o DM since 10 yrs.
K/c/o HTN since 10 yrs
Not a k/c/o asthma, TB, epilepsy, thyroid .
No surgical history.
O/E :-
Patient was c/c/c ,
No pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy,edema.
Vitals:-
Temp: 100.2 F
Bp : 130/70 mm hg
PR: 18 BPM
Spo2 :- 99% @ RA
Grbs: 261 gm/dl
Cvs:- S1,S2 heard, no murmurs .
Rs:- BAE present,
Wheeze in left IAA present.
p/A:-
Obese, mild tenderness in lower abdomen in left hypochondrial religion.
CNS:-
Patient was conscious,
Speech - normal
No signs of meningeal signs.
Provisional diagnosis:-
Acute Gastro enteritis with acute bronchitis with DM and HTN.
Treatment:-
1. IVF NS, RL @ 150 ml/ hr.
2. Inj. Metrogyl 400 mg , iv/ tid.
3. Inj. Pantop 40 mg iv/od
4. Inj. Zofer 4 mg iv/ sos
5. Neb. Budecort and duolin 6 th hrly.
SOAP
Day 2:-
SOAP
Day 2
Subjective:-
Patient complains of fever , vomitings .
Objective-
Pt c/c/c ,
Febrile - 104.2 F
Bp : 140/60 mm hg
PR: 98bpm
RR : 22 cpm
Cvs : S1,S2 present.
Rs:-wheeze present in left IAA .
P/A:-
Soft, Mild tenderness present in right hypochondrium and epigastric reigion.
CNS :-
HMF intact.
Assessment:-
Acute GE with HTN and Dm - 2 with acute bronchitis.
Plan :-
1. IVF - RL , NS @ 150 ml/hr.
2. Inj. Metrogyl 400mg iv/od
3. Inj. Pantop 40 mg Iv/od
4. Inj. Zofer 4 mg iv/sos.
5. Tab. Sporolac - Ds po/od
6. Tab. Pcm 650 mg po/tid
7. Neb.with budecort and duolin 6 th hrly.
8. Inj. Monocef 1 gm iv/bd.
SOAP
Day 3
Subjective:-
Fever , vomitings -- resolved.
Pain abdomen present.
Objective-
Pt c/c/c ,
Febrile - 104.2 F
Bp : 140/70 mm hg
PR: 102bpm
RR : 22 cpm
Cvs : S1,S2 present.
Rs:-wheeze present in left IAA .
P/A:-
Soft, Mild tenderness present in right hypochondrium and epigastric reigion.
CNS :-
HMF intact.
Assessment:-
Acute GE ( resolved)with HTN and Dm - 2 with acute bronchitis.
Plan :-
1. IVF - RL , NS @ 150 ml/hr.
2. Inj. Metrogyl 400mg iv/od
3. Inj. Pantop 40 mg Iv/od
4. Inj. Zofer 4 mg iv/sos.
5. Tab. Sporolac - Ds po/od
6. Tab. Pcm 650 mg po/tid
7. Neb.with budecort and duolin 6 th hrly.
8. Inj. Monocef 1 gm iv/bd.
SOAP
Day 4
Subjective:-
Fever , vomitings -- resolved.
Pain abdomen present.
Shortness of breath +
Objective-
Pt c/c/c ,
Febrile - 99.7 F
Bp : 140/80 mm hg
PR: 118bpm
RR : 34 cpm
Spo2. : 100% on 4L of
Cvs : S1,S2 present.
Rs:-wheeze present in left IAA .
P/A:-
Soft, Mild tenderness present in right hypochondrium and epigastric reigion.
CNS :-
HMF intact.
Assessment:-
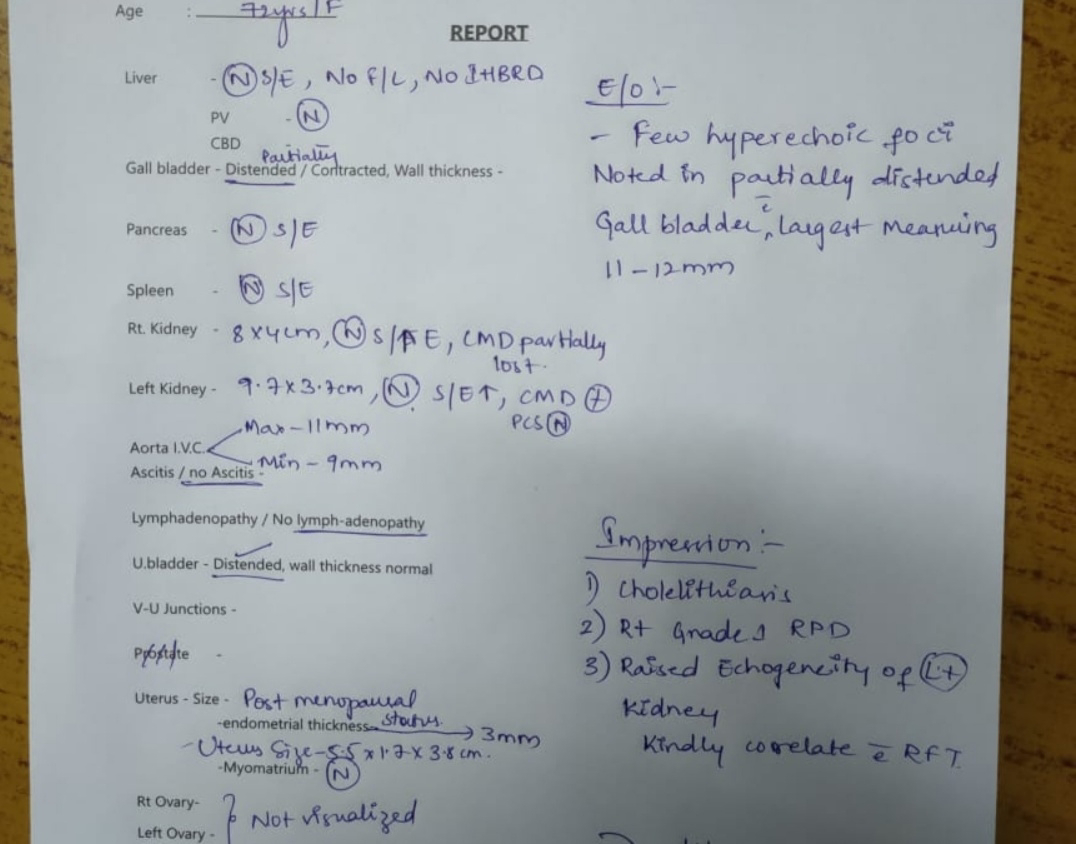
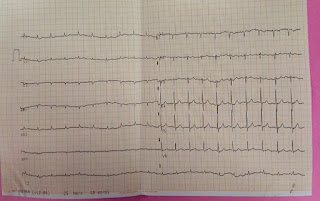
Sepsis secondary to ?CAP with HTN and DM -2 (uncontrolled) with acute bronchitis with paroxysmal AF.
Plan :-
1. IVF - RL , NS @ 150 ml/hr.
2. Inj. Metrogyl 400mg iv/od
3. Inj. Pantop 40 mg Iv/od
4. Inj. Zofer 4 mg iv/sos.
5. Inj. Hydrocortisone 100 mg iv/bd.
6. Tab. Pregabalin 75 mg po/od.
7. Neb.with budecort and duolin 6 th hrly.
8. Inj. Meropenam 1 gm iv/bd .
9.Inj. Lasix 40 mg iv/bd .
10. Bp, temp, and Grbs charting .
SOAP
Day 5
72year woman
She says she is feeling better
Her dyspnea has reduced but
Has been feeling feverish since morning
Patient is conscious, cooperative
PR - 100bpm
Heart rate - 72bpm
Apex pulse deficit of 28bpm
BP - 170/100mmhg
RR - 30bpm
Temp - 100.5 F
Spo2 - 90 % on RA
I/0 - 2700/1500
Stool - passed
Per abdomen - soft
Non tender
Lungs - left side inspiratory crepts in left mammary, IAA, ISA
CVS - S1,S2 +
She was started on insulin infusion on Sunday night, currently her GRBS is 172mg/dl made her infusion to 1ml/ hour as her
Abg yesterday -
PH - 7.4
Pco2 - 21.1
Po2 - 106
Hco3 - 12.9
Anion gap -21.9
Tapered her off inotropic support
A - sepsis secondary to ? CAP with HTN
With uncontrolled sugars, known case of type 2 DM
With acute bronchitis
Paroxysmal AF
P -
O2 inhalation to maintain spo2 -<94%
IVF - RL, NS @ 75ml/hour
Inj Meropenam 1gm/IV/BD day 3
Inj Metrogyl 400mg/IV/TID day 6
Inj Lasix 40mg/IV/BD
Tab Atorvas 20mg/HS
Tab Diltiazem 30mg /PO/TID
Tab Pregabalin 75mg PO HS
SOAP
Day 6
72year woman
She says has been feeling fever since last night
Patient is conscious, cooperative
PR - 125bpm
BP - 130/70mmhg
RR - 30bpm
Temp - 101 F
Spo2 - 98 % with 15L of oxygen
I/0 - 1400/1000
Per abdomen - soft
Diffuse tenderness
Lungs - left side inspiratory crepts in left mammary, IAA, ISA
CVS - S1,S2 +
GRBS - 204mg/dl
A - Sepsis secondary to ? CAP with HTN
With uncontrolled sugars, known case of type 2 DM
With acute bronchitis
Paroxysmal AF (resolved)
CHADVAS score - 2
P -
O2 inhalation to maintain spo2 -<94%
IVF - RL, NS @ 75ml/hour
Inj Insulin infusion at 2ml / hour
Inj Meropenam 1gm/IV/BD day 4
Inj Metrogyl 400mg/IV/TID day 7
Inj Unfractionated heparin 5000Units/IV/TID
Inj Lasix 40mg/IV/BD
Tab Atorvas 20mg/HS
Tab Diltiazem 30mg /PO/TID
Tab Pregabalin 75mg PO HS
Nebulization with Ipravent 2nd hourly
Budecort 6th hourly











Comments
Post a Comment